

New approach to reduce antibiotic dependency against diseases
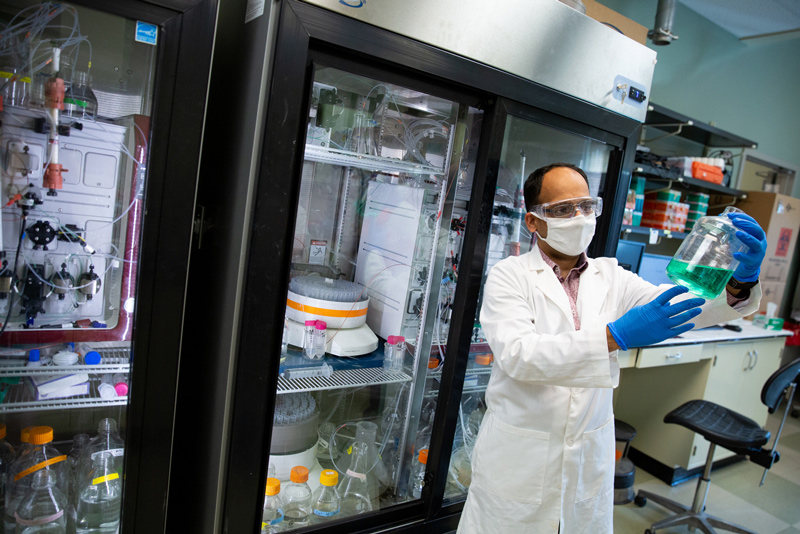
Photo by Ashley Barnas April 07, 2022
UD professor identifies keys for interrupting bacterial communication to prevent infections
As the challenges of confronting bacterial infections and viruses become increasingly prevalent, University of Delaware Professor Vijay Parashar and his team use biochemistry, structural biology and molecular genetics to investigate the mechanisms bacterial proteins use for pathogenesis — the development of disease within the body.
The human body consists of trillions of bacterial cells. Vijay Parashar, assistant professor in the Department of Medical and Molecular Sciences, has dedicated his research to studying these bacterial cells to effectively understand how they become infectious and opportunities to alter the communication pathways involved.
“Our long-term goals are to understand and intervene in the bacterial communication processes,” Parashar said. “Signaling pathways operate like electrical circuits, and if we can determine how certain proteins turn on these circuits, we can learn how to control or modify them. This can help manufacturers design drugs that modify bacterial behaviors, instead of relying on antibiotics against disease.”
Parashar’s research article, published in the Journal of Biological Chemistry, explores how a recently discovered second messenger in bacterial cells helps a cell to respond to an environment similar to that during host infection. This second messenger, bis-(3’,5’)-cyclic diadenosine monophosphate, known as c-di-AMP for short, is responsible for various behaviors of bacterial cells such as virulence, antibiotic resistance and DNA damage repair. Within a cell, this second messenger binds to a universal stress protein, setting forth the events for the development of an infection.
Determining protein structure at an atomic resolution
To better understand the functions of universal stress proteins, Parashar and his team explored these structures at the level of a single atom using powerful tools such as macromolecular crystallography and functional analyses.
“We’ve been taking 3-D ‘pictures’ of these proteins at a resolution scale of nanometers, allowing us to see the protein’s atomic structure to ultimately guide how it functions in the cell,” Parashar said.
Staphylococcus aureus, the bacteria that causes multi-drug-resistant Staph infections, is otherwise part of normal human microflora. It is known that the second messenger c-di-AMP regulates function of the universal stress protein and likely the severity of Staph infections in the human body. Parashar’s laboratory used crystallography to discover how and exactly where c-di-AMP binds to the S. aureus universal stress protein.
“By determining the touch points where these molecules meet, there is great potential for designing drugs that can interfere in these signaling events leading to virulence,” Parashar said. “Ultimately, this can prevent the bacterial cells from becoming infectious.”
Mitigating the consequences of antibiotics
The use of antibiotics is widely accepted throughout the medicinal world but comes with various risks and long-term concerns.
“The issue is that antibiotics are designed to kill most bacterial cells within the body including the good ones, which can lead to an assortment of potential side effects,” Parashar said. “Not only that, an immense survival pressure from antibiotics also forces bacterial cells to adapt and develop resistance against these drugs. To us, it may only be an infection, but to the bacteria, it is a matter of survival. Unfortunately, this has significantly reduced antibiotic effectiveness over time.”
Instead, Parashar and his team see potential in targeting specific infectious behaviors of bacteria. One such promising approach is to control the bacterial ability to sense and respond to their environment.
“By targeting the underlying inter- and intra-cellular communication events, bacterial cells could be prevented from becoming pathogenic in the first place,” Parashar said. “This novel class of anti-infectives would not kill bacteria, thus reducing survival pressure. In turn, this would prevent resistance development against these agents in the long run."
An additional challenge in developing anti-infectives is limited understanding of bacterial communication events.
“We’re laying the foundation for this using one protein at a time,” Parashar said. “However, there are many other pathogenic bacteria that contain similar proteins serving identical functions. Therefore, these same principles can be applied across different bacteria.”
Also, new drugs fail when they are not designed to specifically hit a particular surface in a protein’s structure. The availability of high-resolution 3-D structures, such as universal stress proteins, further facilitates this understanding and paves the way for highly accurate structure-guided drug development.
Looking forward, Parashar and his team aim to further explore how these signaling pathways work within bacterial cells and continue to better realize how they can be modified to prevent diseases.
This research is funded by the National Institutes of Health’s Outstanding Investigator Award, New Jersey Health Foundation Inc., Rutgers Translational Science and a BUSCH Biomedical Grant.
Contact Us
Have a UDaily story idea?
Contact us at ocm@udel.edu
Members of the press
Contact us at 302-831-NEWS or visit the Media Relations website

