

Novel nanomedicines
Photos by Kathy F. Atkinson | Illustration by Joy Smoker October 10, 2023
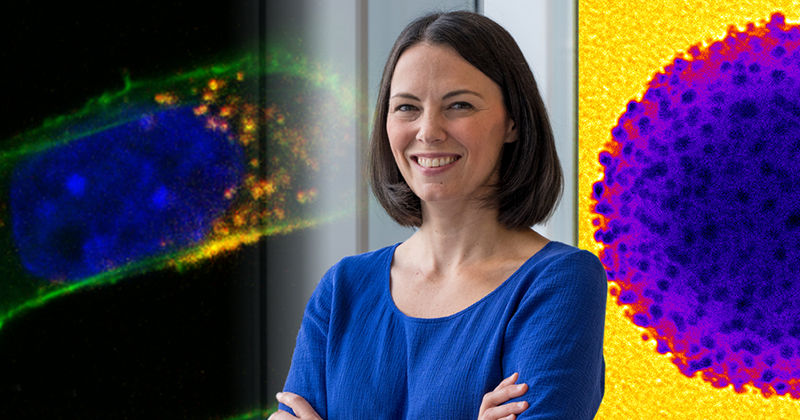
Professor Emily Day is developing therapies to improve outcomes for difficult-to-treat conditions
For the nearly 2 million Americans who will receive a cancer diagnosis each year, treatments like surgery and chemotherapy can be effective but also challenging to recover from. Because of the severity and side effects of currently available cancer treatments, researchers are working on new strategies for these and other difficult-to-treat diseases. These include new ways to deliver drugs directly to a tumor or tissue, meaning that a lower dose can still be effective without causing unintended harm to healthy tissues.
Here at the University of Delaware, associate professor Emily Day is conducting research on these types of high-precision therapies. Now, thanks to an R35 grant from the National Institutes of Health (NIH), Day’s group will continue its innovative research on designing, characterizing and using unique nanoparticles to manage diseases including cancers, blood disorders and reproductive health conditions.
At the forefront of nanomedicine
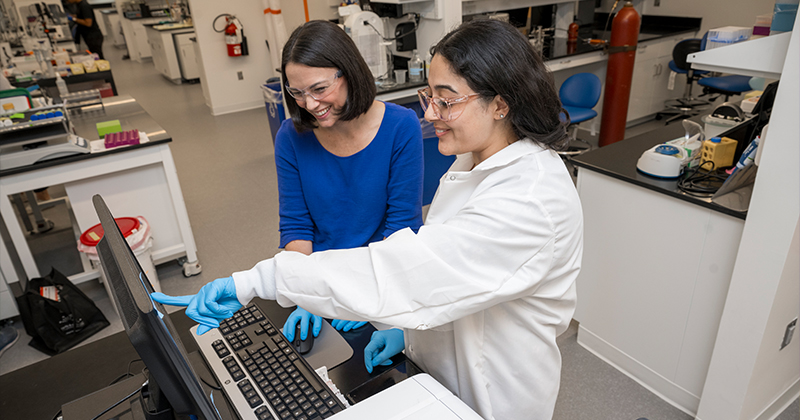
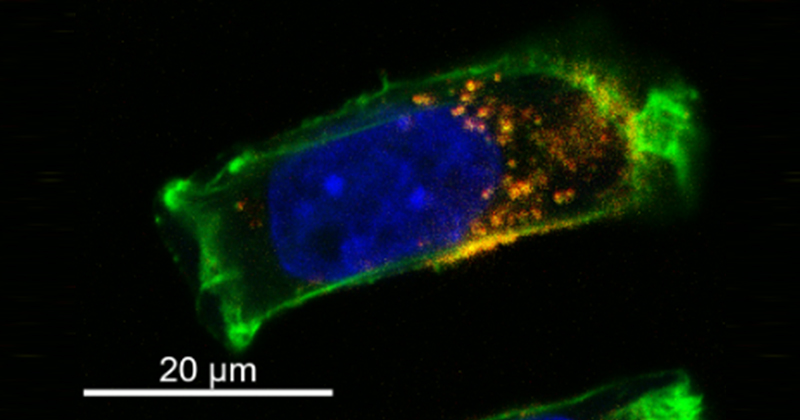
The Day Lab develops nanomaterials that have unique physical and chemical properties that allow them to evade detection by the immune system, target specific cells in the body, and deliver therapeutic cargo. Day’s team precisely designs the structure and surface chemistry of its nanoparticles and performs mechanistic studies to understand how these materials interact with cells and tissues once they are inside the body. The lab’s long-term goal is to improve how different diseases are studied, diagnosed and treated.
What makes her group unique in the nanomedicine field, Day said, is the lab’s ability to “span the spectrum from the fundamentals to the applications.” In other words, to both make unique materials in the lab while also thoroughly exploring how they could be used in the clinic.
“We have a lot of expertise developing bio-nanoconjugates, which are nanoparticles that are coated with biological materials like antibodies or cell membranes,” Day said. “Our team is very good at thoroughly characterizing the systems we make in the lab. This allows us to probe structure-function relationships and gain insights into why the nanomaterials are working the way they are.”
While the team’s research primarily takes place in the pre-clinical setting, the long-term goal of the lab is to improve disease treatment paradigms — or “get medicines where they need to go with high precision,” Day said. To achieve this goal, Day said it is critical to understand structure-function relationships, as this will allow for the development of improved nanomedicines.
“Over the past decade, we have found that nanoscale architecture is critical to nanomedicine performance. For example, we’ve seen that antibody nanocarriers are dramatically more effective than freely delivered antibodies because they can engage multiple receptors on a diseased cell simultaneously, which increases binding strength to yield better therapeutic effects,” she said. “Overall, we’ve found that it’s not just what you deliver, but how you deliver it that really matters.”
Multidisciplinary strategies
Along with the lab’s research on cancer, Day’s group also works on treatments for blood disorders and gynecological conditions. In the lab, researchers use a variety of treatment strategies and analytical tools to begin to address the many questions that remain unanswered in their field.
One treatment strategy involves using nucleic acids or antibodies to inhibit genes that are implicated in disease progression. In this area, doctoral candidate Elise Hoover is developing antibody-targeted, polymer-based nanoparticles to treat an especially aggressive form of breast cancer (triple-negative breast cancer, or TNBC). Her research involves finding ways to target Wnt signaling, a key developmental signaling pathway that cancer cells “hijack” so they can grow and spread.
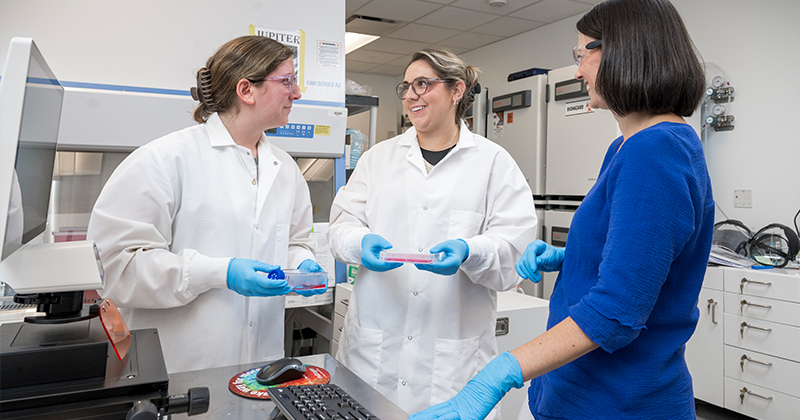
“Using antibodies, I target a specific receptor that’s part of the Wnt signaling pathway,” Hoover said. “Then, I deliver either a chemotherapeutic drug, a small interfering RNA [siRNA; a gene expression suppressor] or both using the antibody-targeted polymer nanoparticles.”
Doctoral candidate Mackenzie Scully also works in this area and is focused on reducing the overexpression of beta-catenin (a “master regulator” of Wnt signaling that allows cancer cells to grow and spread uncontrollably) in TNBC using siRNA knock-down techniques.
“One goal of my project is to assess whether our particle coatings can effectively increase the uptake of the nanoparticles by targeted cells while maintaining low uptake by non-targeted cells,” Scully said. “Then, once the nanoparticles are inside diseased cells, we then determine if they can release enough cargo to cause a desired level of gene or protein suppression.”
While Hoover uses nanoparticles coated with antibodies to provide cell-specific targeting, Scully coats her nanoparticles with membranes taken from the surface of cancer cells. This process places the unique lipids and proteins that are within the membrane onto the nanoparticles, which allows them to evade immune detection and bind to other cancer cells in the body.
Sara Aboeleneen, another doctoral candidate in the Day Lab, also tries to improve the targeting of nanoparticles to tumors by wrapping them with cancer cell membranes for another treatment strategy known as photothermal therapy. Here, when the nanoparticles are delivered to a tumor, they are irradiated with tissue-penetrating, near-infrared light, which causes them to convert the light into heat to kill the cancer cells.
“I’m trying to improve the targeting of these particles to the tumor by wrapping them with cancer cell membranes,” said Aboeleneen, who is conducting fundamental research to see if these membrane-wrapped nanoparticles can provide more efficient photothermal therapy of TNBC than non-targeted nanoparticles.
Working outside of TNBC treatment strategies, Eric Sterin, also a doctoral candidate, is evaluating ways to use this membrane-wrapping technique for treating blood disorders. With the goal of using nanoparticles to deliver therapeutic cargo to blood stem cells, Sterin is first studying how the nanoparticle’s surface chemistry changes in the presence of proteins found in the blood.

Because these proteins bind to nanoparticles (resulting in a protein corona) and make them easier to clear from the body, understanding this process is essential.
“I'm trying to understand the immune response to membrane-wrapped nanoparticle systems and why they get taken up and cleared from the body — essentially, what is happening to the nanoparticles from the immune system side so we can minimize that effect,” he said.
Breaking down barriers
In support of her trailblazing research, Day recently received an R35 grant, also known as a Maximizing Investigators' Research Award (MIRA), from the NIH. The grant’s five years of funding is designed to provide researchers with the stability and flexibility to pursue interesting findings as they are discovered so they can achieve breakthroughs more quickly.
“This grant will allow us to perform studies aimed at understanding and overcoming biological barriers to nanoparticle delivery,” Day said. “Once a particle is administered into the body, it encounters a lot of barriers — it must evade recognition by the immune system, penetrate vascular and/or tissue barriers, interact with the right cells in the tissue, and deliver the cargo in the right time and location without causing off-target toxicity. What we want to do is use the particles we've already made for other projects to investigate questions related to these biological barriers and come up with ways to improve delivery across those barriers.”
Two initial research questions they will be addressing thanks to this funding include protein corona-mediated immune clearance, or how proteins bound to nanoparticles influence their distribution in the body, and how nanoparticles cross blood vessel walls, specifically how inflammation impacts blood vessels and downstream particle delivery to specific tissues.
If they can find ways to overcome these biological barriers, it could lead to “a huge shift in the clinical impact of nanomedicine,” Day said. “If we can figure out how to overcome these barriers, it will translate to a greater ability to effectively treat more diseases.”
Fundamental research with far-reaching impacts
While the research in their lab is fundamental, Day said that the implications of their findings could potentially impact many types of conditions.
“Because we perform fundamental research, the discoveries we make could be very broadly applicable to the field of nanomedicine,” Day said. “The structure-function relationships we define could ultimately be expanded to enhance the performance of particles that people are developing all across the globe.”
As one example, Sterin said that membrane-wrapping research, which uses similar building blocks as the mRNA COVID vaccines, could help prevent treatments from being cleared from the body before they can reach their targets.
“It would be really cool to develop a way to have these treatments be more effective, to not get cleared out of the body, and define a mechanism that could also be used in lipid nanoparticles so they could become more ubiquitous delivery systems,” Sterin said about the broader implications of his research.
Scully added that because this membrane-wrapping technology is still relatively new, there are still clinical limitations to address before it can be fully adopted into treatments.
“We envision that someday researchers could take a tumor biopsy, extract the membranes off a patient’s own cells, and put them on nanoparticles to provide a personalized medicine,” she said. “Alternatively, if we can make that process more allogeneic, similar to how blood transfusions work, then it could be applicable to an even larger group of people. However, there are FDA-related clearances you need to complete to ensure these processes are safe.”
Aboeleneen hopes her research can help light-activated nanoparticles be used in more clinical trials in the future. Nanoparticle-mediated photothermal therapy has already shown promise in clinical trials, but she hopes her approach to improve the targeting of the nanoparticles to tumors can “make a difference in people's lives,” she said.
For Hoover, who has family and friends who have undergone treatments for cancer, working on fundamental ways to improve cancer treatment helps motivate her.
“People get excited when I tell them what I’m working on, and that helps me get more excited that my work could improve someone’s life,” she said. “Overall, it would be great to see these targeted therapies become more commercially available, not just for cancer but for other diseases as well. We’re a targeted nanomedicine lab, and that targeting is crucial for new treatments going forward.”
Contact Us
Have a UDaily story idea?
Contact us at ocm@udel.edu
Members of the press
Contact us at 302-831-NEWS or visit the Media Relations website

