Clotting problem
Photo courtesy of UD's Fowler Lab | Illustration by Jeffrey C. Chase March 06, 2020
UD-led team uncovers a blood disorder’s creeping, crawling origin
Ouch, you’ve cut your finger! As you fumble to grab a tissue, the paramedics in your blood are already rushing to the scene. These blood cells, called platelets, morph in shape from round to spiny, sticking to each other and to the injured blood vessel walls, to begin patching the gash. The platelets join together with other proteins to form a mesh-like plug—a clot—to stop the bleeding.
But for the 1 in 25,000 people estimated to have MYH9-related disorders, caused by mutations in the MYH9 (myosin) gene, their blood doesn’t clot so well, resulting in a range of health issues—kidney failure, heavy menstrual periods, cataracts, hearing loss.

What’s at fault? In research published in Blood, the journal of the American Society of Hematology, University of Delaware Professor Velia M. Fowler and her collaborators at UD and the National Institutes of Health reveal a number of wrong moves by blood cells on their creeping, crawling journey toward platelet formation.
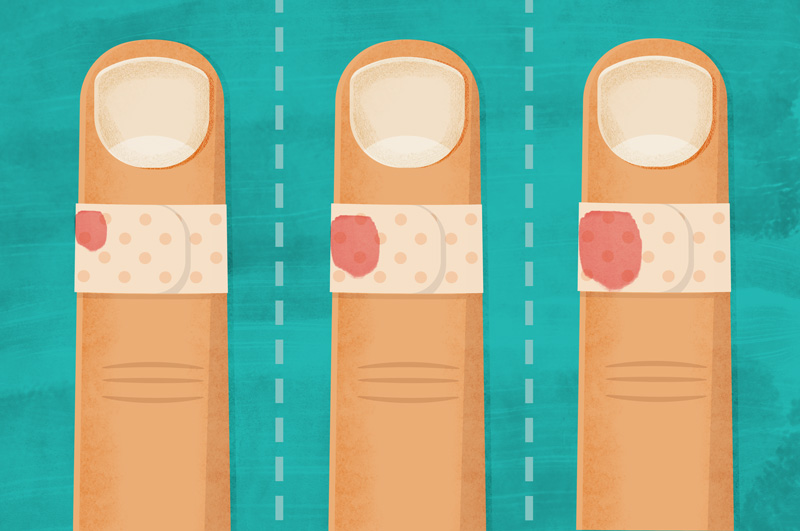
While platelets normally are tiny, less than one-tenth the size of red blood cells, and the average person generates some 40 billion of these clotting cells a day, people with MYH9-related disorders have scant numbers of them. What’s more, their platelets are jumbo-sized and can even be as big as red blood cells.
“In people with MYH9-related disorders, the platelets are few and they are just way too big,” said Fowler, professor and chair of UD’s Department of Biological Sciences. “They look like bluish giants in our stains under the microscope.”
Studying cells from mice that mimic the human disease, Fowler and her team began looking for defects in the platelet-making process. Platelets originate from humongous cells called megakaryocytes, which, in turn, are derived from stem cells, in the soft, gelatinous marrow at the center of your bones. These megakaryocytes creep and crawl from the bone marrow to neighboring blood vessels—the sinusoids—which have leaky walls that allow other cells to squeeze through. This is where the megakaryocytes extend branch-like arms called proplatelets into the blood vessel, and the circulating blood shears them off into many small platelets.
“Megakaryocytes are really, really large cells that glide forward pulling their large cell body along behind them like a snail dragging its shell,” Fowler said. “They use proteins like myosin and actin, which regulate muscle contractions, to move from here to there in a process called cell motility.”
How the cells know to go in a certain direction is still somewhat a mystery, Fowler said, but involves the ability of the megakaryocyte to sense chemoattractant molecules released from the blood vessels, similar to a dog following a scent.

The team tracked and filmed these megakaryocytes during their migration from bone to blood vessel. Their focus was three mouse-cell lines, each representing a different known mutation in the myosin-9 protein molecule (for which the MYH9 blood disorder is named).
Using an inverted microscope, which allows researchers to view and film samples of live cells from below rather than from the top down, the researchers recorded the direction and distance these megakaryocytes traveled. When they plotted the data, they could see that the mutant cells were all going in the wrong direction like a pack of bloodhounds that had lost their sense of smell.
“They have lost their way somehow, but we don’t really know why,” Fowler said.
The mutant cells also move in erratic ways: too slowly or too randomly or much faster than they should, sometimes almost in a hyper state.
“The megakaryocyte cells can’t get there—to the blood vessel—so you can’t get platelets,” Fowler said, “but the reason they can’t get there is different for each mutation.”
Specifically, cells with the R702C mutation experience a loss of myosin contractility—the ability of their microscopic muscle-like cellular structures to contract—making them too slow; cells with the D1424N mutation gain greater contractility resulting in rapid and at times hyperactive movement; and cells with the E1841K mutation produce contractility at random.
Based on these findings, Fowler said, personalized drug therapies and treatments would be needed to enhance or reduce the cells’ directionality and movement issues, depending on the patient-specific mutation.
“Just as megakaryocyte migration properties are affected by improper MYH9 myosin function, it is also possible that clots formed by the platelets carrying these mutations are unstable,” Fowler said. “Further hematological analysis of platelet properties from MYH9-RD patients will be required to determine if these mutations affect clot formation. Since many patients with MYH9-RD also develop cataracts, hearing loss and kidney problems, our study can also shed light on the causes for other defects associated with this disease in patients.”
Fowler, who began this study at the Scripps Research Institute, where she worked prior to joining the UD faculty in 2019, has nothing but praise for her research team, including the first author on the paper, Kasturi Pal, a former postdoctoral researcher at UD.
“Dr. Pal was just fantastic—she had never worked with megakaryocytes before. But she is one of these people who takes risks, initiates collaborations and responds to constructive criticism,” Fowler said. “I’m proud to have had a role in mentoring her.”
Pal recently began a new position as assistant professor of biological sciences at Ashoka University in Sonepat, Haryana, India.
Other co-authors include Roberta Nowak, senior research associate at Scripps Research Institute; Neil Billington, structural biologist, Rong Liu, L’Enfant Postdoctoral Fellow, and James Sellers, senior investigator, all from NIH’s National Heart, Lung and Blood Institute; and postdoctoral researcher Arit Ghosh from UD.
The research was supported by NIH National Heart, Lung and Blood Institute (NHLBI) grant R01-HL083464 to Fowler, NHLBI Division of Intramural Research support to Sellers (ZIAHL001786) and a Judith Graham Pool National Hemophilia Foundation postdoctoral fellowship to Pal.
Contact Us
Have a UDaily story idea?
Contact us at ocm@udel.edu
Members of the press
Contact us at mediarelations@udel.edu or visit the Media Relations website