

Delivery of medicine in the body
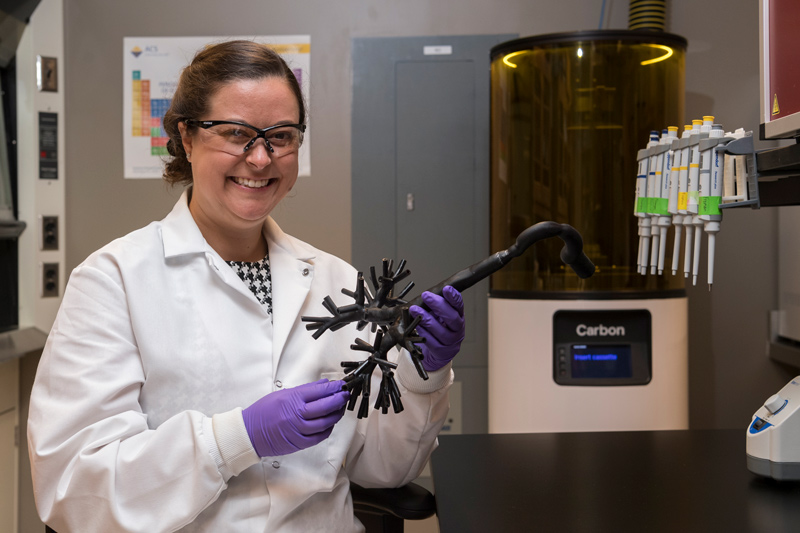
Photo by Kathy F. Atkinson October 01, 2021
UD Prof. Catherine Fromen will use moving models to study how medicines travel in the lungs and gut
The human body has built-in protections to keep pathogens out.
That sneezing fit or stuffy nose when you have a cold? That’s your body leveraging mucosal linings in your respiratory system to expel the offending virus.
But these natural defenses also sometimes work to keep out medicines, a challenging problem that has hindered treatment solutions for diseases such as cancer, fibrosis and even COVID-19.
University of Delaware chemical engineer Catherine Fromen wants to better understand how these organ-protection mechanisms work to improve the delivery of therapeutic medicines to the body.
Fromen has been awarded a $2 million grant from the National Institutes of Health (NIH) Maximizing Investigator’s Research Award program, which provides promising early-stage investigators with sustained funding to pursue novel ideas.
The five-year MIRA grant will support core areas of Fromen’s work focused on designing medicines that go to mucosal interfaces, such as inhalable vaccines for respiratory problems. She is particularly interested in knowing where these medicines need to go to overcome mucosal barriers, say in the lungs or the gastrointestinal tract, to better interact with immune cells.
“By better understanding how mucus and cells behave at these mucosal barriers, we can better design methods and medications to treat different problems at these protective barriers,” said Fromen, an assistant professor in the Department of Chemical and Biomolecular Engineering.
UDaily caught up with Fromen to learn about her plans for advancing this work.
Q: What are mucosal interfaces, and why are they so important to human health?
Fromen: Mucosal interfaces are found in the human body’s respiratory, gastrointestinal, reproductive and urinary systems. These are the sites where we are most vulnerable and where pathogens infect first. Unique immune cells there can act independently from the body’s overall immune system to produce region-specific responses to any foreign invaders. If we can deliver medicines directly to these cells at the front line, then we can think about improving the barrier protection and fighting off pathogens. With the lung, this could be solutions for diseases like lung cancer or infectious disease like COVID-19 or influenza. In the gut, this could be celiac disease, which is an improper immune (autoimmune) response to the gluten found in certain foods.
Q: How do mucosal barriers work, and how do we want them to work better?
Fromen: The body’s immune system is often thought of like an army, where each of the different cell types have different military functions. You can think of the mucosal interface like the walls of a castle, with foot soldier cells patrolling the castle and lookout cells searching for trouble on the horizon. Either of these cells can go inside the castle and say, “Mount up; it's time” and direct the body’s response to different problems.
These immune cells spend a lot of time at this protective layer waiting for the right signal to do something. If we can flip a switch here, it can create a whole cascade of events to do something totally different that benefits the whole organ or patient.
Q: Can you share an example?
Fromen: Sometimes these cells have been trained incorrectly to be overprotective in a way that has unintended side effects. Maybe cells at this mucosal interface are supporting a tumor cell and they shouldn’t be — can we give instructions to alert the immune cells that the tumor cell is bad, so that they wake up and do all the things they are normally good at doing?
Currently, we are only able to deliver single-word instructions so those cells can marshal the troops to perform complicated actions. We need to be able to get better, more frequent messages to these cells.
Q: Where will you begin?
Fromen: We will initially focus on the lung since that’s an area of expertise for my lab. However, the work is more broadly applicable to mucosal interfaces in other places like the human gut because both organs are in constant motion and have a huge surface area.
In previous work, my lab created a 3D-printed lung model that incorporates the tissue’s unique branched architecture. We plan to add motion to our model and run fluids and medicines through it to figure out how the system works at a fundamental level. Researchers have studied on a small-scale how mucous flows left to right or how things diffuse through it, but no one has looked at the bigger transport mechanisms — the thickness of the mucus, how long things can stay in one place, how things change. We want to see the lung moving as it creates air and the mucus on top of it, to study how medicines move through this macroscopic framework, even before they hit the mucus.
Q: What will this tell you?
Fromen: One of the biggest challenges we face from a pharmaceutical standpoint is not knowing where the medicine goes once inside the body. We can build simulation models to explore things like how medicines diffuse to the tissue when we put it at specific branches of the lung, but we don’t know how to predict, effectively, where it goes inside the entire organ or how long it will stay there. The same is true in the gut. We can estimate, but each body is different.
Additionally, most studies and simulations of how medicines move within the body assume a healthy person of a particular body weight. This can be problematic, since we know that a person’s lungs can appear incredibly different depending on smoking status, age or weight. Currently, however, there is no way to incorporate this information into predicting how medicines will work. That’s where our model comes in.
Q: Why is it important to be able to study this movement?
Fromen: Even something as simple as making the epiglottis — that little flap in your throat that covers the esophagus when you swallow — open or close is challenging. But this is a real pinch-point for inhaling medicines, so even a model with just a little motion could provide important information on how medicines move or disperse under various conditions, for example, short, shallow breaths versus longer, deeper breaths.
Q: What other questions do you plan to address?
Fromen: The other side of the work focuses on understanding what happens when the medicine gets where it is going. We need to unravel how the medicine’s formulation design interacts with specific immune cells that live at the mucosal barrier. We have interesting data that these cells can live for longer by taking up foreign objects (medicines, viruses) and that their lifespan at the mucosal interface is regulated by frequency of these interactions.
These sentinel cells are critical in taking outside information and coordinating tissue response. We want to explore whether, by changing the chemistry of the formulation of inhaled medicine, we can turn knobs to control what these immune cells are doing and for how long, to create a desired effect.
Q: Where do you hope this work will lead?
Fromen: There is so much disease that originates at this mucosal interface, so it’s a real opportunity to improve human life. Think about vaccines … if we can better understand how to deliver medicines to treat cells directly at the site, it will be even better than getting a shot in the arm. I’d love to see what we are making become therapeutic products that end up FDA approved to help patients with respiratory issues in my lifetime, or see our models used to screen therapeutics and advance personalized medicine.
Contact Us
Have a UDaily story idea?
Contact us at ocm@udel.edu
Members of the press
Contact us at mediarelations@udel.edu or visit the Media Relations website

