- Rozovsky wins prestigious NSF Early Career Award
- UD students meet alumni, experience 'closing bell' at NYSE
- Newark Police seek assistance in identifying suspects in robbery
- Rivlin says bipartisan budget action, stronger budget rules key to reversing debt
- Stink bugs shouldn't pose problem until late summer
- Gao to honor Placido Domingo in Washington performance
- Adopt-A-Highway project keeps Lewes road clean
- WVUD's Radiothon fundraiser runs April 1-10
- W.D. Snodgrass Symposium to honor Pulitzer winner
- New guide helps cancer patients manage symptoms
- UD in the News, March 25, 2011
- For the Record, March 25, 2011
- Public opinion expert discusses world views of U.S. in Global Agenda series
- Congressional delegation, dean laud Center for Community Research and Service program
- Center for Political Communication sets symposium on politics, entertainment
- Students work to raise funds, awareness of domestic violence
- Equestrian team wins regional championship in Western riding
- Markell, Harker stress importance of agriculture to Delaware's economy
- Carol A. Ammon MBA Case Competition winners announced
- Prof presents blood-clotting studies at Gordon Research Conference
- Sexual Assault Awareness Month events, programs announced
- Stay connected with Sea Grant, CEOE e-newsletter
- A message to UD regarding the tragedy in Japan
- More News >>
- March 31-May 14: REP stages Neil Simon's 'The Good Doctor'
- April 2: Newark plans annual 'wine and dine'
- April 5: Expert perspective on U.S. health care
- April 5: Comedian Ace Guillen to visit Scrounge
- April 6, May 4: School of Nursing sponsors research lecture series
- April 6-May 4: Confucius Institute presents Chinese Film Series on Wednesdays
- April 6: IPCC's Pachauri to discuss sustainable development in DENIN Dialogue Series
- April 7: 'WVUDstock' radiothon concert announced
- April 8: English Language Institute presents 'Arts in Translation'
- April 9: Green and Healthy Living Expo planned at The Bob
- April 9: Center for Political Communication to host Onion editor
- April 10: Alumni Easter Egg-stravaganza planned
- April 11: CDS session to focus on visual assistive technologies
- April 12: T.J. Stiles to speak at UDLA annual dinner
- April 15, 16: Annual UD push lawnmower tune-up scheduled
- April 15, 16: Master Players series presents iMusic 4, China Magpie
- April 15, 16: Delaware Symphony, UD chorus to perform Mahler work
- April 18: Former NFL Coach Bill Cowher featured in UD Speaks
- April 21-24: Sesame Street Live brings Elmo and friends to The Bob
- April 30: Save the date for Ag Day 2011 at UD
- April 30: Symposium to consider 'Frontiers at the Chemistry-Biology Interface'
- April 30-May 1: Relay for Life set at Delaware Field House
- May 4: Delaware Membrane Protein Symposium announced
- May 5: Northwestern University's Leon Keer to deliver Kerr lecture
- May 7: Women's volleyball team to host second annual Spring Fling
- Through May 3: SPPA announces speakers for 10th annual lecture series
- Through May 4: Global Agenda sees U.S. through others' eyes; World Bank president to speak
- Through May 4: 'Research on Race, Ethnicity, Culture' topic of series
- Through May 9: Black American Studies announces lecture series
- Through May 11: 'Challenges in Jewish Culture' lecture series announced
- Through May 11: Area Studies research featured in speaker series
- Through June 5: 'Andy Warhol: Behind the Camera' on view in Old College Gallery
- Through July 15: 'Bodyscapes' on view at Mechanical Hall Gallery
- More What's Happening >>
- UD calendar >>
- Middle States evaluation team on campus April 5
- Phipps named HR Liaison of the Quarter
- Senior wins iPad for participating in assessment study
- April 19: Procurement Services schedules information sessions
- UD Bookstore announces spring break hours
- HealthyU Wellness Program encourages employees to 'Step into Spring'
- April 8-29: Faculty roundtable series considers student engagement
- GRE is changing; learn more at April 15 info session
- April 30: UD Evening with Blue Rocks set for employees
- Morris Library to be open 24/7 during final exams
- More Campus FYI >>
10 a.m., Oct. 1, 2009----More than 60 percent of adults and 20 percent of children in the United States are overweight or obese, a condition that threatens not only their physical health but also their emotional well-being.
“A lot of effort has been directed at the problem of obesity,” says Steven Most, assistant professor in the Department of Psychology at the University of Delaware. “There's a great deal of information available about eating right and exercising, but that's only half the battle. Access to healthy alternatives works only as far as individuals actively choose to pursue them.”
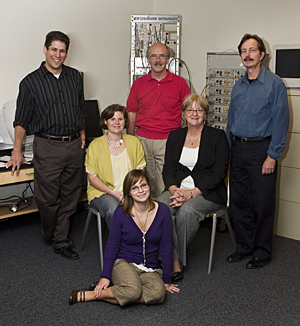
In a new approach to this multi-faceted and seemingly intractable problem, Most is partnering with Dr. Sandra Hassink, director of the Pediatric Weight Management Clinic at A.I. duPont Hospital for Children; Meredith Lutz Stehl, a clinical psychologist at the hospital; and James Hoffman and Robert Simons, professors in UD's Department of Psychology. Their collaborative research is aimed at assessing whether individuals struggling with weight management exhibit characteristic neuro-cognitive indices related to attentional control and self-control.
The team hopes to answer a number of questions that explore the response of obese people to food stimuli, as this information may help in designing and implementing effective interventions.
For example: Do individuals struggling with weight management exhibit marked impulsiveness or difficulties involving attention shifting, working memory, and behavior inhibition? Are weight management problems accompanied by exaggerated responses to food cues and/or by a relative inability to regulate such responses? Do common food cues, such as pleasant aromas, have a negative impact on cognitive control functions?
The developmental project is one of 15 supported by Delaware's INBRE (IDeA Networks of Biomedical Research Excellence) program, which is funded by a five-year, $17.4-million grant from the National Institutes of Health (NIH). The projects are aimed at generating preliminary data to support the development of subsequent research proposals to NIH and other funding agencies.
Introducing direct measures of attention and response to food stimuli is a novel way to approach an individual's decision-making around food choices. According to Simons, while issues like impulsiveness and attentional control have been investigated using paper-and-pencil measures, these self-reports are subjective and they don't allow the various components of complex concepts like “attention” to be isolated. So the team plans to combine behavioral testing with the use of direct measures known as event-related brain potentials (ERPs).
The study will compare ERPs from a subject population of overweight adolescents undergoing treatment at the A.I. Weight Management Clinic, as well as from a control group matched for age, sex, and socioeconomic status. An initial battery of tests will assess baseline attention, working memory, and self-control processes. A second series of tests will measure neural indices of arousal and reflexive attention to food-related visual and olfactory cues, as well as the subjects' ability to override and regulate such responses.
In one test, for example, subjects are shown a collection of pictures and asked to locate the one depicting a particular item, say a chair, as quickly as possible. The question here is whether the presence of enticing food pictures in the mix will slow down the ability of the weight-management subjects to find the designated item.
The project protocol will enable the researchers not only to compare the two populations but also to assess changes in the obese population over time as they progress through the treatment program.
“This study represents an exciting new area to explore,” Hassink says. “The more we understand the process of decision making about food choices, the more effective we will be at helping our patients.”
Most emphasizes the importance of the collaboration with clinicians at A.I. duPont. “Drs. Hassink and Lutz Stehl bring a very important level of expert knowledge to this project,” he says, “and the clinic will serve as an incredibly and uniquely rich source of participants.”
Such collaborations are becoming more commonplace as a result of the Delaware Health Sciences Alliance (DHSA), a coalition launched in March 2009 to provide leadership in health and health services. A partnership of Christiana Care Health System, Nemours, Thomas Jefferson University, and the University of Delaware, the DHSA is aimed at improving the health of local residents with cutting-edge research and enhanced healthcare education.
“This project exemplifies the type of interdisciplinary biomedical research that we have been fostering under the INBRE grant,” says Karl Steiner, associate provost for interdisciplinary research initiatives and INBRE program coordinator. “This collaboration among academic and clinical experts from UD and A.I. duPont further strengthens the growing relationship under the Delaware Health Sciences Alliance.”
Most and Hoffman are both cognitive psychologists, and Simon's previous work has focused primarily on anxiety disorders, so working in the area of obesity is new for all three. “We're just at the beginning of trying to understand these mechanisms,” says Hoffman, “but I think there's evidence that disorders like this involve defects in basic cognitive functions.”
If Hoffman is right, the research may lead to more effective weight loss programs for both children and adults. “We already know that most cases of obesity result from people consuming too much food and getting too little exercise,” Most says. “But if we want to change those behaviors, we have to figure out the neuro-cognitive mechanisms that are behind them so that we can retrain the brain.”
Article by Diane Kukich
Photo by Ambre Alexander


